Dr Mohit Mandiratta, was born and raised in Birmingham. He is a GP Partner and GP trainer at Black County ICB. You may have also seen him on BBC Breakfast and on twitter @DoctorMoMan.
Be proactive on health

“Our communities don’t tend to speak about conditions like cancer and the importance of checking our bodies,” says Dr Mandiratta.
“Many people delay getting help, even when they need advice and some people with cancer keep it a secret because they feel ashamed or don’t want to burden anyone. We need to get better at recognising the warning signs and talking about it.
“A family history of cancer may put you at higher risk, which is another reason to tell our loved ones. And when we catch it early, cancer is easier to treat and your chance of recovery is higher.”
Although testicular cancer isn’t common, it affects men between the ages of 15 and 49 years. Regularly checking the size and weight of testicles, as well for swelling or lumps will help to identify when something’s wrong.
Breast cancer also affects men over the age of 60 and sometimes younger. Although rarer, it’s important men check their chest, armpit and collarbone area for anything unusual, including new lumps, changes to skin texture or the size or any discharge from the nipple.
“Though it can feel strange to do this, it’s important you’re familiar with how your body feels. If you have a sudden or ongoing pain, a lump that wasn’t there before or unexplained bleeding, these should be checked by a healthcare professional,” adds Dr Mandiratta.
“If you have symptoms you can’t explain or that are worrying you, you should contact your GP practice. These include coughs lasting over three weeks, blood in your urine or stools, or a change in a mole or a persistent sore.
“Often, it’s nothing to worry about and you’ll have peace of mind. But we want to detect problems early on so if it is serious, we can help you get appropriate treatment sooner.”
Grab your jab: There is still time to have the first two doses of the COVID-19 vaccine. COVID-19 is still here, but your vaccination will help to protect you and your loved ones from serious illness.
NHS health screening – your MOT

“I always advise my patients and friends to take-up the offer of the range of NHS screening programmes,” Dr Mandiratta, “It helps to identify health risks and signs of disease they might not see or feel.”
NHS screening can help identify if you’re at risk of serious health problems. This includes:
• Bowel cancer screening – everyone aged 60 to 74 will be sent a home testing kit, called a Faecal Immunochemical Test (FIT kit for short), in the post by the NHS. This is gradually being expanded to include people aged 50 to 59. People aged 75 and over can also request a kit, which is used to collect a tiny stool sample to be analysed for traces of blood that could be a sign of bowel cancer.
• Abdominal aortic aneurysm (AAA) screening - offered to men aged 65 and over, who are most at risk. Using an ultrasound, this checks for a bulge or swelling in the aorta, the main blood vessel from the heart through the tummy. If an aneurysm bursts, it can be life-threatening.
• Diabetic eye screening for those aged 12 years and over who have diabetes. It checks for eye problems which can lead to sight loss if not found early.For more information about these and other NHS screening programmes, visit www.nhs.uk
Other common tests
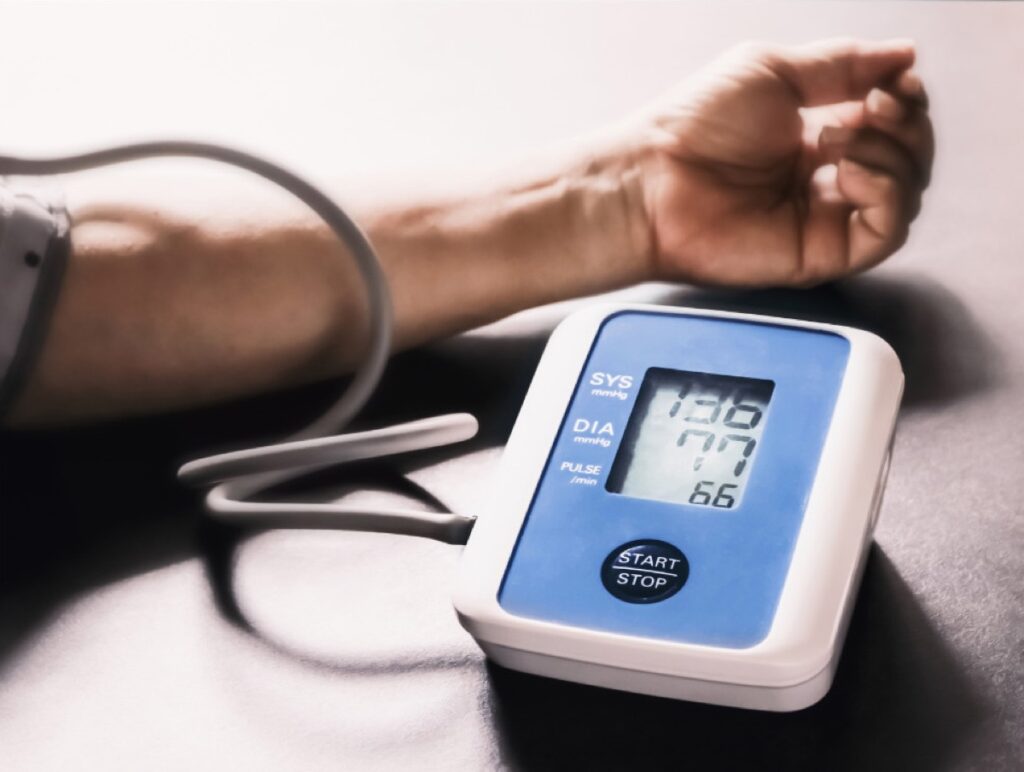
• In the UK around 5 million people have high blood pressure without knowing it, and people of South Asian heritage are at higher risk. It often has no symptoms and can increase your risk of heart attack or stroke. Free blood pressure checks are available in some pharmacies, your GP practice and as part of the NHS health check for the over-40s. “High blood pressure is treatable. Your GP practice can advise you about diet, exercise and treatment,” says Dr Mandiratta.
• You might also be offered a blood test to measure your cholesterol. This is a type of fat which can build up in the arteries, increasing your risk of a heart attack or stroke.
• A man’s risk of developing prostate cancer increases with age, and men over 50 or who have a family history of prostate cancer can request a prostate-specific antigen (PSA) blood test from their GP. This measures levels of a protein which can be raised if you have prostate cancer. But it’s important to discuss results with your doctor because a raised level doesn’t necessarily mean you have cancer. Prostate cancer usually doesn’t have symptoms in its early stages, but if you need to urinate more often, have blood in your semen or urine, are straining or have a stinging or burning sensation when urinating, or notice changes to your urine flow, wake at night to pass urine or your bladder feels like it isn’t emptying fully, you should seek advice from your GP as soon as possible. Check your risk for prostate cancer with the Prostate Cancer UK risk checker.
A healthy mind and body

There is a lot we can do as individuals, families and communities to improve our mental and physical health:

• Eat a balanced diet to help prevent or manage type 2 diabetes, which is more common in South Asian communities and if left uncontrolled, can have life changing consequences. But there are ways to eat the foods we love, while reducing sugar, salt and unhealthy fats to reduce the risk.
• Get active, take at least 150 minutes of moderate intensity (or 75 minutes vigorous intensity) physical activity each week. If you’re over 65, being physically active every day is recommended. Fresh air is great for doing low-impact activities that are great for your joints, such as walking or cycling. But if it’s cold outside, you might prefer to go to swimming, or even being active at home. Activities such as yoga or Pilates will help build your strength but you won’t need lots of equipment to enjoy them. Speak to your GP practice for advice if you have medical conditions or any concerns.
• Get your vaccines, vaccines help to build your immunity against serious illness. In addition to COVID vaccination, you might also be invited for a flu jab each year, if you are aged over 50, have a long term condition, are pregnant or are a frontline NHS or social care worker. At the age of 65, you are entitled to a Pneumococcal (PPV) vaccine, which some call the pneumonia vaccine, and a shingles vaccine for people in their 70s. Find out more at nhs.uk/vaccinations
• Quit smoking and tobacco, all forms of tobacco are bad for us and increase our risk of cancer. This includes smoking cigarettes, bidi and shisha, as well as chewing tobacco like paan and gutkha. You’re more likely to quit with support and you can get free expert advice and encouragement from professionals at Find your local Stop Smoking Service.

• Reduce your stress, make relaxation part of your daily routine, whether it’s meditation, mindfulness, massage, or creative activities. Find out about calming breathing exercises and other advice that might help at www.nhs.uk
• Connect with people for emotional support, if you’re struggling with feelings of anxiety or depression, one of the most important things we can do is to speak to someone about it. That can be a family member, friend, neighbour, or religious leader.
• Speak with a healthcare professional if your thoughts, feelings or behaviour are affecting everyday life. Your GP may suggest NHS talking therapies and you can also refer yourself via www.nhs.uk/talk. The NHS also offers a range of mental health services and can also put you in touch with other organisations that can help.
You can book your COVID-19 vaccination at nhs.uk/COVIDvaccine, by scanning the QR code, or by calling 119. You can find out more about the NHS services at www.nhs.uk/nhs-services
















