
Although bowel cancer is the fourth most common type of cancer, and the UK’s second biggest cancer killer, many people feel uncomfortable talking about their bowel habits, explains Dr Anisha Patel.
“I’m a mother of two and a GP from Surrey, so being diagnosed with stage 3 bowel cancer at the age of 39 was a real shock.

“I’m fit and healthy, I don’t have a family history of cancer and don’t have any risk factors. But I‘m sharing my story to help others recognise symptoms of bowel cancer – so they can get help sooner.”
What is bowel cancer?
The large bowel is part of our digestive system which helps to absorb water from our food, as well as remove food waste from our bodies. Bowel cancer can affect any part of the large bowel, including the colon and rectum.
It’s not always clear why a person gets bowel cancer, but genetic changes, environment and lifestyle factors may play a part.
Dr Patel tells us: “You may be more likely to get bowel cancer if you’re overweight, smoke or have a close relative who has had it. People who have an inflammatory bowel disease (like Crohn’s disease or ulcerative colitis) or bowel polyps may also be at a higher risk.”
Every year, 42,900 new cases of bowel cancer are diagnosed in the UK, with 2,600 of these in people under the age of 50. “Even though 90% of cases are people aged over 50, I know first-hand that it can affect anyone, of any age,” she adds.
Can I prevent it?
Although bowel cancer isn’t preventable, leading a healthier lifestyle can reduce our risk of getting bowel cancer. “Following these simple tips can help to lower our risk from many conditions, such as type 2 diabetes as well as bowel cancer” explains Dr Patel.
“Eating a healthy diet with plenty of fruits, vegetables and fibre, eating less red and processed meat and staying active with regular exercise is recommended. You can also get help to quit smoking, reduce your alcohol intake and to lose weight if you need to.”
You can find out more and download apps at: www.nhs.uk/better-health
What symptoms should I look out for?
If we know what our normal bowel habits are, we can spot when something doesn’t feel right.
Dr Patel explains: “Not everyone’s habits are the same, so we should listen to our bodies. Keep an eye on how regularly you go and check your stools for their shape and consistency. Also keep an eye out for any blood in the toilet or tissue before you flush.”
Symptoms we should look out for include:
• changes in your stools, such as having softer stools, diarrhoea or constipation
• needing to go to the toilet more or less often
• blood in your stools, which may look red or black
• bleeding from your bottom
• often feeling like you need to go to the toilet, even if you’ve just been
• tummy pain and/or bloating
• losing weight without trying
• feeling very tired for no reason
“As a doctor, perhaps I played down my symptoms. Initially I had bloating, cramps and sometimes felt an urgency to go to the toilet, which I put down to irritable bowel syndrome (IBS).
“I occasionally saw blood on the toilet paper, which I thought could be due to a pile as I gave birth a few years before. I felt very tired, but as a mum of two young children, running a household and being a GP, I didn’t find it unusual.

“But as my symptoms got worse including my bowel movements, I finally went to see my GP.
“My stools became thin and ribbon-like because there was a tumour obstructing it, so the signs may not always be obvious. After some scans and tests, I was referred for specialist treatment and diagnosed with bowel cancer.”
Dr Patel urges people not to feel embarrassed about talking to their doctor if they have symptoms they are concerned about. “If you feel uncomfortable talking about your bowel movements or worries, please remember we’re used to examining all parts of the body and hear about things like this all the time.
“So please come to see us if you think something doesn’t feel right. It’s particularly important to contact your GP practice if you have had symptoms for three weeks or more. It might not be cancer – but you need to know.”
If your stools are black or dark red or you have bloody diarrhoea, book an urgent appointment with your GP practice or call NHS 111 for free. If you’re bleeding non-stop from your bottom or there’s lots of blood in the toilet (e.g. the water turns red or you see large blood clots), you should go to A&E or call 999.
What is bowel cancer screening?
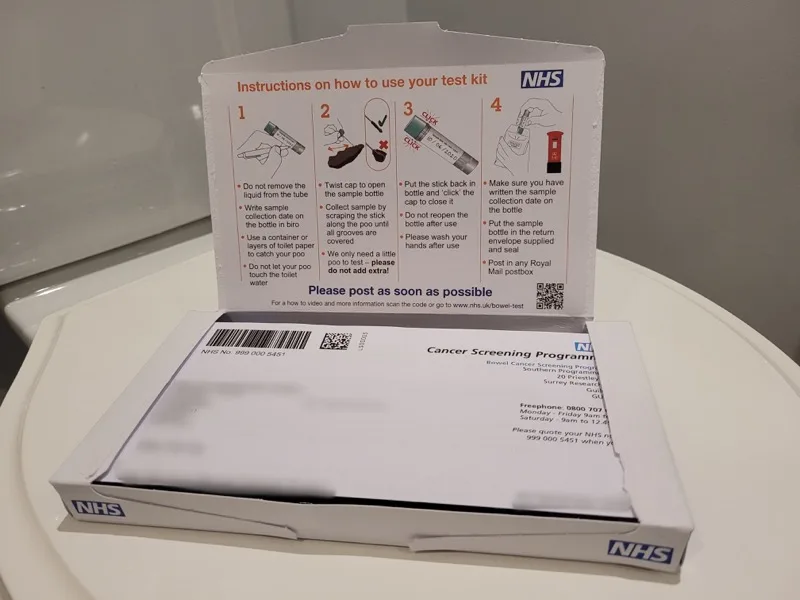
Eligible people aged 60-74 years old are invited to take part in the NHS bowel cancer screening programme every two years, using a home testing kit called a Faecal Immunochemical Test (or ‘FIT kit’ for short). The programme is currently expanding to also include 50-59 year olds too, so you may get a test before you’re 60.
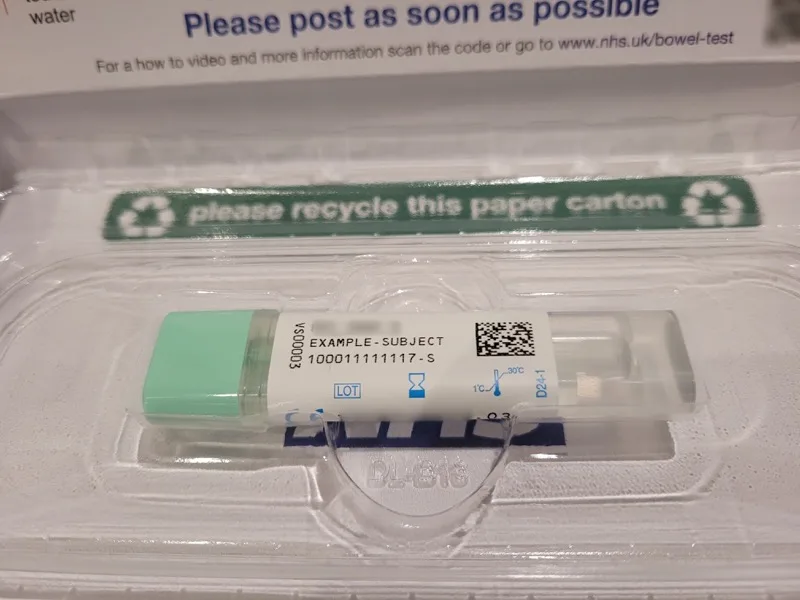
You use the kit at home and take a small sample of your stool, which you put into a tube and post back to the NHS. It’s then tested for small traces of blood, a possible sign of cancer, that are not visible by eye. The presence of blood doesn’t mean you have bowel cancer, but further tests such as a colonoscopy are usually advised.
Dr Patel says: “If you or anyone in your family gets a test kit through the door, I plead with you – don’t put it off. It takes just a moment but can help spot cancer even if you don’t have any obvious symptoms.”
About 98% of people who use their bowel cancer screening kit do not need further tests. 2% are asked to go to hospital for further tests. Just under 10% of those people who go to hospital for further tests will be diagnosed with cancer. However, a further 55% will have polyps found during their hospital procedure. Polyps are not cancer, but may develop into cancer over time. Polyps can be easily removed during a colonoscopy and reduces the risk of bowel cancer developing.
“If bowel cancer is diagnosed early, it’s treatable and can be curable. The test really can save your life,” says Dr Patel.
The ongoing expansion to also include eligible people aged 50-59 years means annually, around 4.2 million more people will be eligible for the NHS bowel cancer screening programme. This means that when the full rollout has been completed, the total eligible population will be more than nine million people each year. You can find out more at www.nhs.uk/conditions/bowel-cancer-screening.
How I dealt with my diagnosis
“Anyone who has ever had the misfortune of receiving life changing news will know how I felt – hopelessly lost, distraught, and directionless, and at other times inconsolably upset, angry, and irritated.
“I was scared as I went in for the operation to remove the tumour. I didn’t know what I was going to wake up to. Would the cancer be gone? Would I need chemo-radiotherapy?
“Thankfully, my tumour was removed completely and I had three months of chemotherapy to reduce the risk of the cancer returning.
“With the help of my GP, specialists, nurses, online support groups and my network of family and friends, I have tried to turn this negative situation into a positive. I share my story to raise awareness of bowel cancer and to help alleviate the stigma surrounding this cancer. If you have symptoms, don’t delay seeing your GP practice – early diagnosis saves lives.”















